Hypospadias Surgery Explained: Everything You Need To Know
Key Takeaways:
- Hypospadias is a common congenital condition affecting 1 in 200 to 1 in 300 male births, requiring surgical intervention for optimal outcomes.
- It presents in three main forms: glandular, penile, and perineal hypospadias, each with varying implications for function and appearance.
- The causes of hypospadias are multifactorial, involving both genetic predispositions and environmental factors during fetal development.
- Hypospadias can have significant medical and psychological impacts, necessitating a holistic treatment approach that includes psychological support.
- Preparation for surgery includes thorough consultations with specialists, adhering to preoperative guidelines, and managing anxiety for both parents and children.
- Surgical techniques for hypospadias repair include onlay or tubularized incised plate (TIP) techniques and the preputial flap technique, chosen based on severity.
- Post-operative care is vital, involving monitoring for complications, pain management, and adherence to care guidelines to facilitate healing.
- Long-term follow-up is important for assessing healing and managing potential complications, including psychological impacts related to body image.
- Building support systems and open communication within families can enhance resilience and emotional well-being during recovery and beyond.
Diving Deep: What is Hypospadias and Why Does It Matter?
Hypospadias is a congenital condition characterized by an abnormality in the male urethra where the opening is not located at the tip of the penis, but instead can be found anywhere along the shaft or even at the base. Understanding hypospadias is crucial because it not only affects the physiological aspect of urination and sexual function but can also influence psychological development and self-esteem in boys as they grow. Hypospadias is estimated to occur in about 1 in 200 to 1 in 300 male births, highlighting its prevalence and the importance of medical intervention. Due to variations in severity and type, each case of hypospadias requires careful consideration, individualized assessment, and tailored surgical treatment to ensure the best outcomes for the affected child.
The Anatomy of Hypospadias: Variations and Implications
Hypospadias manifests in various forms, categorized primarily based on the location of the urethral opening. The three main types include glandular, penile, and perineal hypospadias. Glandular hypospadias is the mildest form, where the meatus (urethral opening) is located near the tip of the penis. Penile hypospadias presents a more significant deviation, as the meatus is positioned anywhere along the shaft. Perineal hypospadias represents the most severe manifestation, with the urethra opening found near the scrotum. Each of these anatomical variations comes with specific clinical implications, impacting both function and aesthetic appearance, though surgical repair can typically restore normalcy. Understanding these variations is essential for parents and medical professionals, as it helps tailor the approach to treatment, ensuring effective management of any resulting complications such as urinary tract infections, infertility issues, or psychological impacts stemming from body image concerns.
Unraveling the Causes: Genetics and Environmental Factors
The precise cause of hypospadias remains a subject of ongoing research, but evidence suggests a multifactorial origin involving both genetic predispositions and environmental influences. Genetic factors may involve specific chromosomal anomalies or inherited traits that increase the likelihood of the condition. Meanwhile, environmental factors—such as maternal exposure to certain medications, chemicals, or conditions during pregnancy—may also play a role. Hormonal imbalances during critical periods of fetal development are believed to be influential as well. Understanding these causative factors is vital for medical professionals and parents alike, as it assists in counseling families about potential future occurrences in siblings and informs preventive strategies when planning for subsequent pregnancies.
Understanding the Impact: Medical and Psychological Perspectives
The implications of hypospadias extend beyond clinical concerns, intersecting with psychosocial development. Medically, individuals with hypospadias may face complications such as urinary issues, infections, or complications from surgical procedures. However, psychological impacts can be profound, particularly for boys aware of their condition as they grow. Treatments and surgeries are not purely technical; they also focus on the relational and emotional aspects of the individual, emphasizing bodily autonomy, self-esteem, and acceptance. It’s crucial for healthcare providers to adopt a holistic approach, ensuring they incorporate psychological support in therapeutic regimens—such as counseling—to promote a positive self-image and social integration, further enriching the patient’s overall quality of life.
Preparing for the Big Day: What to Expect Before Hypospadias Surgery
Preparation for hypospadias surgery is a multi-faceted endeavor, requiring meticulous planning and open communication between parents, patients, and medical teams. The primary goal is to ensure that both parents and the child feel informed and secured leading up to the surgical intervention, thereby improving outcomes and reducing anxiety.
Consultations and Evaluations: Choosing the Right Specialist
Choosing the right specialist is a fundamental step in the journey toward hypospadias repair. Pediatric urologists trained specifically in these procedures are best suited to address the intricacies of hypospadias. During initial consultations, parents should expect thorough evaluations including physical examinations and diagnostic imaging if necessary to understand the anatomy clearly. It’s vital to ask questions about the surgeon’s experience, techniques employed, and the expected outcomes based on the individual child’s case. Secondary consultations with specialists in genetics or psychology may also be beneficial, providing a holistic understanding of potential impacts on the child’s future. Establishing a sense of trust and collaboration with the healthcare team can play a pivotal role in alleviating concerns and ensuring that parents and patients are thoroughly prepared for surgery.
Preoperative Guidelines: Setting the Stage for Success
Adhering to preoperative guidelines is essential for maximizing surgical success and minimizing complications. Typically, this includes dietary restrictions, such as fasting prior to surgery, and possible medication adjustments. Parents should receive detailed instructions on bathing and grooming in the days leading up to the procedure, as cleanliness is crucial in reducing the risk of infection. Preoperative assessments may also comprise blood tests and a review of the child’s medical history to evaluate any potential anesthetic risks. Preparing emotionally is equally important; parents should consider discussing surgical expectations with their child using age-appropriate language for understanding resilience and cooperation during recovery. This preparation process helps ensure the child feels comfortable and secure when the day comes, fostering a sense of control over the situation.
Managing Anxiety: Tips for Parents and Patients Alike
Anxiety surrounding medical procedures is common, especially for young children and their families. Parents can play an essential role in managing anxiety by maintaining a calm demeanor and addressing the child’s concerns openly. Engaging in pre-surgery activities like storytelling can help normalize the experiences associated with hospital visits. Parents should also familiarize their child with the surgical environment, emphasizing positive aspects like friendly staff and toys in waiting rooms. Techniques such as deep breathing and visualization can be introduced to children, enabling them to cope with their fears. Involving the child in the preparatory discussions and decisions can also empower them, supporting their emotional coping mechanisms. For parents, it can be helpful to seek support from counselors, support groups, or other families who have gone through similar experiences, reinforcing the understanding that they are not alone in this journey.
The Surgical Journey: What Happens During Hypospadias Repair?
The hypospadias surgical procedure is an intricate process that requires the coordinated effort of a skilled surgical team, focusing on rectifying anatomical abnormalities to restore normal function and appearance.
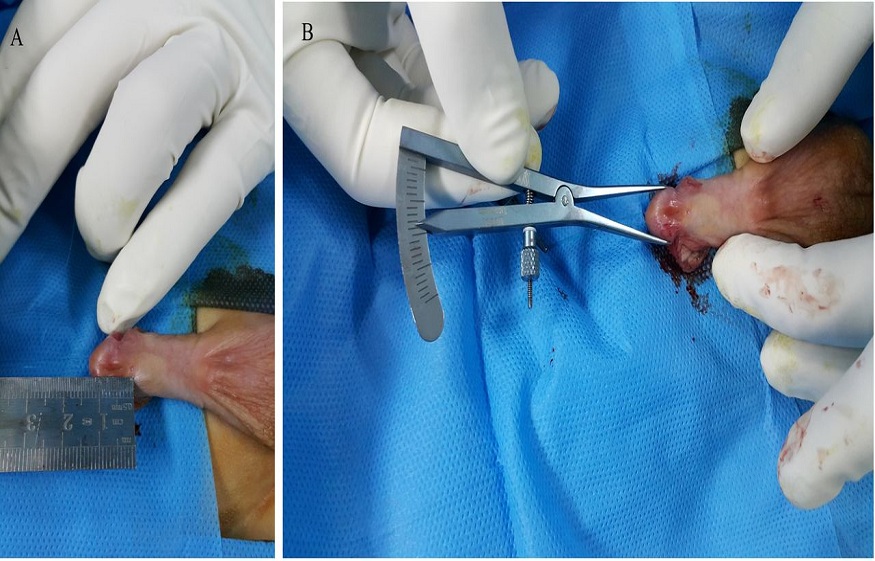
Types of Surgical Techniques: Finding the Right Approach
Two primary approaches to hypospadias repair are the onlay or tubularized incised plate (TIP) techniques and the preputial flap technique. The choice of technique depends on the severity of the hypospadias and the surgeon’s expertise. The TIP procedure involves creating a new urethral channel using tissue from the penis and is typically used in cases of mild to moderate hypospadias. In contrast, the preputial flap technique employs skin from the foreskin—when available—to create a new urethral opening, preferred for more complex cases. Each method has distinct advantages and potential drawbacks, thus necessitating a comprehensive discussion between parents and surgeons to reach an informed decision tailored to the child’s unique condition.
A Step-by-Step Walkthrough: From Anesthesia to Recovery
Surgery typically begins with the administration of general anesthesia, ensuring that the patient is fully unconscious and pain-free during the procedure. Following anesthesia, the surgeon makes a small incision to access the urethra. Once the abnormal opening is identified, the existing urethral channel is either restructured or recreated using the surrounding tissue or grafts from other areas if needed. After meticulous reconstruction, the area is closed with sutures, and a catheter may be placed to facilitate urine drainage while healing occurs. Post-surgery, the child is moved to a recovery area where they are monitored closely as they wake from anesthesia. Parents are usually allowed to be present to comfort and reassure their child during this transition, contributing to a smoother recovery experience. Nurses play an integral role during this phase, providing vital observations and intervention if any signs of complications arise.
Addressing Common Concerns: Risks and Challenges
As with any surgical procedure, there are risks involved in hypospadias repair, including complications such as bleeding, infection, and issues with healing or urethral stricture. Parents should be informed about potential signs of complications to watch for, including unusual swelling, persistent pain, or discharge. Long-term outcomes have largely been favorable for most children; however, it’s vital to acknowledge that some may face challenges as they grow, including the need for additional surgical interventions, particularly if complications arise or if there are concerns about functional aspects, such as urinary flow or sexual function. Comprehensive pre- and post-operative education for parents is essential in managing expectations and preparing them to support their child holistically throughout the surgical journey.
The Road to Recovery: Navigating Post-Operative Care and Beyond
The recovery phase following hypospadias surgery is a critical time that requires careful attention to ensure proper healing and favorable outcomes. Parents play a vital role in facilitating this journey, ensuring adherence to care guidelines while also supporting their child’s emotional and physical needs.
Understanding Healing: What to Expect in the Days Following Surgery
In the days following surgery, it is common for parents to observe swelling and tenderness in the surgical area. Regular monitoring for any signs of infection or complications is crucial at this stage. Pain management is a key aspect of recovery; pediatricians typically prescribe medications to alleviate discomfort. It’s essential for parents to follow dosage guidelines accurately and maintain communication with the healthcare team if their child displays unusual symptoms. Encouraging gentle activities while avoiding strenuous play is advisable during this early recovery phase, allowing the child to gradually regain their strength without compromising the surgical site. Education on proper catheter care, if present, is paramount to prevent infections and ensure optimal drainage during recovery.
Long-Term Outcomes: Monitoring Progress and Managing Complications
Monitoring the long-term outcomes of hypospadias surgery involves regular follow-ups with the child’s healthcare provider to assess healing, function, and aesthetic aspects. Most children achieve satisfactory results in terms of both urinary function and appearance; however, follow-up appointments provide an opportunity to address any arising concerns early on. Pediatric urologists often recommend routine consultations into adolescence to monitor sexual development and function. In some cases, additional corrections may be required, but these instances are typically addressed promptly to mitigate long-term effects. Acknowledging potential psychological impacts of hypospadias, including body image concerns or challenges during adolescence, is essential in supporting the child throughout their growth, allowing for timely interventions if needed.
Support Systems: Resources for Families and Patients After Surgery
Building a support system is invaluable for families navigating the complexities of hypospadias surgery. Support groups can provide a safe environment for sharing experiences, concerns, and triumphs with others who understand the unique challenges faced. Online forums and local organizations often facilitate connections among families, fostering collaboration and exchange of resources. Healthcare providers can also refer families to counseling services, assisting with emotional well-being during the recovery period and beyond. Practicing open communication within the family, addressing fears, questions, and milestones together, lays a foundation for resilience. As children transition into adulthood, empowering them to feel comfortable discussing their experiences with trusted individuals can help reinforce a positive sense of identity, promoting acceptance and psychological well-being in the context of their unique journey.
FAQ
Question: What are the potential long-term complications associated with hypospadias surgery? – Long-term complications can include issues such as urethral stricture, problems with urinary flow, or aesthetic concerns regarding the appearance of the penis. Additionally, psychological effects related to body image may arise as the child grows.
Question: At what age is hypospadias surgery typically performed? – Hypospadias surgery is usually performed between 6 months and 18 months of age, although the timing can depend on the child’s specific condition and the recommendations of the healthcare team.
Question: Are there specific symptoms or signs that indicate a complication after surgery? – Parents should monitor for signs of complications such as unusual swelling, persistent pain, redness, discharge from the surgical site, or fever, as these can indicate infection or other issues requiring prompt medical attention.
Question: How can parents support their child emotionally during the recovery period? – Parents can support their child emotionally by maintaining open communication, providing reassurance, engaging in gentle play, and seeking professional counseling if necessary, particularly if the child exhibits signs of anxiety or distress.
Question: Will my child need additional surgeries in the future? – While most children achieve satisfactory results, some may require additional procedures to address complications or concerns that arise as they grow. Regular follow-ups with the healthcare provider are crucial for monitoring.
Question: Can hypospadias affect my child’s sexual development later in life? – Hypospadias can potentially impact sexual function, depending on the severity and the success of surgical repair. Ongoing monitoring and evaluation are important as the child matures.
Question: What role do psychological factors play in the overall treatment of hypospadias? – Psychological factors are significant as they can affect a child’s self-esteem and body image. Including psychological support as part of the treatment plan can help improve the child’s social integration and emotional well-being.
Question: Are there preventative measures for future pregnancies if hypospadias was caused by environmental factors? – While genetic factors cannot be changed, avoiding known environmental risks during pregnancy, such as certain medications and toxins, can be discussed with a healthcare provider to help reduce the likelihood of hypospadias in future pregnancies.






